Modelling and AI helping to improve cancer monitoring
Date:
Changed on 12/12/2019
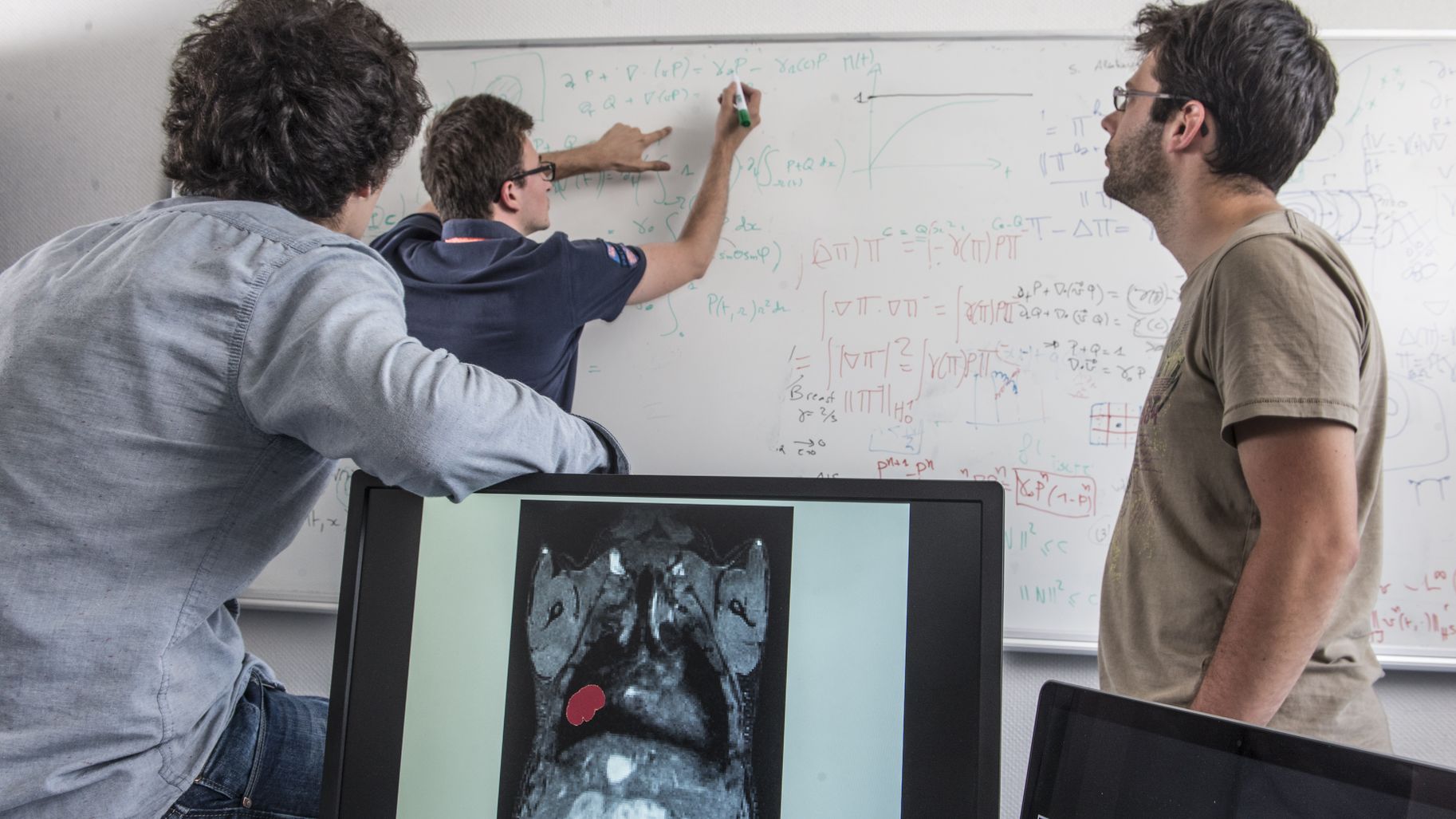
Within our team, we use modelling and artificial intelligence in the fight against cancer. We construct mathematical models capable of describing the progression of the disease, helping us to understand the mechanisms involved in cancer in order to improve follow-up care for patients. We use AI to incorporate parameters or measures that can’t be modelled model into these models or to make a diagnosis directly. We use all of the information available to us: imaging, genomic information, clinical data, etc., the end goal being to assess the effectiveness of a given treatment at an early stage. The idea behind this is to help doctors to work out whether or not the treatment will work a short while after beginning it, enabling them to adapt their treatment strategy accordingly.
We responded to a call for papers from the laboratoryMSD, which were offering 1 million euros’ worth of funding for ambitious research programmes, putting together a project where the aim was to improve follow-up care for patients suffering from non-small cell lung cancer.
It is a very common type of cancer - more than 85% of lung cancers are non-small cell, with 40,000 new cases diagnosed every year. Personalised medicine has revolutionised this disease in recent years. Tumour genomics are now analysed in order to adapt the treatment to the type of tumour. There are different branches of the disease, with a growing number of possible treatments: surgery, chemotherapy, radiotherapy, targeted therapy, immunotherapy, thermoablation and stereotactic radiotherapy. For doctors, choosing the treatment is becoming increasingly complex.
We are trying to stratify patients in order to work out in advance whether or not they will respond well to treatment. Then, once they have started treatment, we will try to work out as quickly as possible whether or not it will work. We take into account all of the routine clinical data that is gathered - and generally not fully used - including imaging and the genomic aspect of the tumour, but also the patient’s biomarkers (including blood samples, for example). This type of data is not easy to correlate with the progression of the disease, but it has the advantage of being available, and it might tell us something.
We are right at the very start - Pimiento was only signed towards the end of 2018. To get things started, we will be focusing on a branch of the disease with which we are already familiar, EGFR mutations, which are generally treated using targeted therapy, tyrosine kinase inhibitors. We will then move on to studying other branches of the disease.
There are 20 of us in the team, all specialists in applied mathematics. We will be hosting two doctors studying PhDs, a radiologist and a nuclear doctor. We have one associate researcher, a nephrologist who works with us on a part-time basis.
We also carry out a significant amount of work alongside doctors. They provide us with the clinical questions, our goal being to answer genuine questions in order to develop useful tools for them to use. They then select the patients and provide the requisite clinical expertise. When we develop an algorithm, we check with the doctors to find out what worked and what didn’t, and what we can improve. We also try to translate doctors’ intuition and expertise into our models. When a radiologist makes a diagnosis, they will have internal criteria that they will often keep to themselves. We try to write this sense of intuition into our models in a quantitative sense, which requires a lot of interaction and discussions with doctors.
We will be supported by Sophia Genetics, a company that specialises in clinical genomics and imaging based on artificial intelligence. As far as hospitals are concerned, we will be working with the Institut Bergonié, in Bordeaux, with whom we have been working for a number of years now. Then there is Hôpital Tenon in Paris (there is a doctor there who studied for his PhD with us) and the Centre Léon Bérard in Lyon. We will be starting off with a small number of centres as we look to build our algorithms, before adding other centres in order to validate our results.